US$325,000,000,000, that’s US$325 Billion, Per Year. Did that number get your attention?
A prominent New York investment bank announced that the addressable market, for one of their IPO clients in 2020, was a managed care/Medicare Advantage Management Services Organization (MSO), valued at $325 billion per year. Today, that public company is “only” doing about US$1B in revenue. According to their latest annual report, they are trading around 15 times the revenue, and earnings before interest, taxes, depreciation, and amortization (EBITDA) of nearly a negative (-) US$230 million. With the public stock very near an all-time high, how can this be?
Well, courtesy of the COVID pandemic, the managed care/Medicare Advantage market has been resurrected from relative obscurity for the past 20 years and is thriving more than ever. The 10,000 persons reaching Medicare eligibility (age 65) daily and upwards of half electing the Medicare Advantage plan route, creating a continuously growing market with a “baked in” 6% CAGR. So, if the $325B had your attention, then perhaps the reports from others that the Medicare Advantage market could be annual $500B by 2028 will.
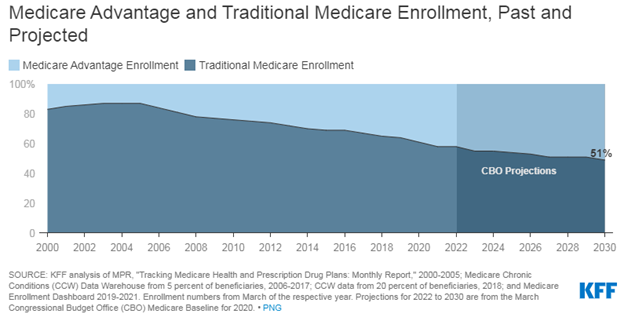
The Congressional Budget Office (CBO) projects that the share of all Medicare beneficiaries enrolled in Medicare Advantage plans will rise to about 51 percent by 2030. See below.
It is not just about revenues. Medicare has created a very consumer driven model where insurance companies both compete for expanding benefits and quality measurements. The “Star” rating system drives consumers to be the best “5 Star” programs – this includes many quantitative and consumer measurements.
We believe Medicare Advantage is the most innovative creation that America could offer to the rest of the world, as the rest of the developed world deals with an aging society. Open, market driven approach with material measurements and consumer information.
When we talk about competition, we’re only looking at our backyard here in South Florida, where a consumer can choose from over 40 individual Medicare Advantage plans offered by a dozen or more companies that range in quality from three (3) stars to five (5) stars, and most refund the consumer or beneficiary their Medicare Part B premium of around $145.00 every month. The growing population of retirees coming to Florida, in addition to those retiring here, creates a thriving market.
COVID has resulted in many physicians trying to deal with the changes in fee-for-service medicine, as opposed to those who are operating or employed by those Medicare Advantage plans and are thriving.
What we believe is missing from the Medicare Advantage business model is not more technology, but better targeted use of technology – not just telemedicine. Increased and enhanced use of Internet of Things (IoT), and even more important, is a unified or universal medical record owned and controlled by the patient. Some big insurance companies have begun exploring development of their own electronic health record (EHR), and one medical service provider that we know of had developed their own EHR. That is rare however, we think it will soon become the norm.
As we have stated and restated, we believe that the line between service and technology will first blurred, then eliminated. This is one of the reasons why we refer to our offerings as “technology-infused healthcare.”
-Noel J. Guillama, Chairman
